The Economics of Insulin Therapy: How the Diabetes Industry Convinced You to Spend More
Today is International Diabetes Day and November is Diabetes "Awareness" Month. Be aware of the economics behind your chosen treatment plan, and choose accordingly.
It’s November 2025 (Diabetes Awareness Month) which means my inbox and social media feeds are flooded with feel-good posts about “diabetes warriors” and corporate platitudes from device companies that often charge $10,000 a year for plastic devices that deliver a $100-a-vial hormone.
I’ve been managing Type 1 diabetes for almost 38 years (since 1-13-1988). I’ve used syringes, pens, and pumps. I’ve dealt with insurance companies, endocrinologists, pharmacy benefit managers (PBMs), and everything in between. I’ve experienced severe hypoglycemia requiring hospitalization (all in college or pre-college) and every minor short-term complication in between. And here’s what nobody wants to tell you: the “best” insulin delivery method isn’t about the latest technology, it’s about what you’ll actually use consistently, afford realistically, and manage responsibly.
This November, instead of the usual diabetes awareness fluff, let’s talk about something that matters: money, outcomes, and the personal responsibility required to beat natural selection when your pancreas doesn’t work.
A critical note before we dive in: Insurance is so F#$%ing complicated that trying to give you accurate “with insurance” pricing is nearly impossible. Every plan is different. Every formulary is different. Every deductible, copay, and out-of-pocket maximum varies. What costs you $50 might cost your neighbor $500 or $5,000 depending on their coverage. So all the prices I’m listing in this post are estimated cash prices – what you’d pay if you walked into a pharmacy or ordered supplies without insurance. Your actual costs will vary wildly based on your coverage, but at least this gives you a baseline to understand what these things actually cost before the insurance shell game begins.
THE DIABETES INDUSTRIAL COMPLEX
First, let’s establish something: the diabetes industry doesn’t want you healthy. They want you compliant. Compliant patients buy more products, need more “support,” and generate more recurring revenue.
The push toward insulin pump therapy over the last two decades hasn’t solely been driven primarily by patient outcomes – though they’ll show you the studies that say it helps. It’s also been driven by profit margins. An insulin pump company makes exponentially more money from a pump patient than Novo Nordisk or BD makes from someone buying a box of pen needles.
Am I saying pumps don’t work? No. I’m saying the conversation around them is not 100% transparent and somewhat dishonest.
Here’s what almost 38 years has taught me: Any insulin delivery method works if you use it correctly. None of them work if you don’t.
Happy Diabetes Awareness Month…
WHAT IT ACTUALLY COSTS
Let me show you numbers that matter, what you’ll actually pay.
Multiple Daily Injections (MDI) – The Reality:
If you’re smart about it, MDI is shockingly affordable. Novo Nordisk, and others, offers programs that make insulin more affordable outside of insurance. Novo’s program allows patients to purchase insulin from their local pharmacy for $99 per month for BOTH your fast-acting and long-acting insulin. That’s $1,188 a year for the stuff that keeps you alive.
Add in syringes or pen needles ($400-600), and basic glucose monitoring ($600-900 for test strips, or $1,200-3,600 if you spring for a continuous glucose monitor), and you’re looking at $2,488 to $5,888 annually depending on your monitoring choice.
Routine endocrinologist visits add another $300-500, which brings the realistic range to $2,788 to $6,388 annually. You may also want to allocate an estimated $8,000 per year for things like hospitalization due to DKA or hypoglycemia, but proper management should keep that risk extremely low.
Total MDI annual cost: $2,788 - $6,388.
Insulin Pumps – The Real Numbers:
Let’s start with the Omnipod 5, which is currently the darling of the diabetes tech world because it’s tubeless and integrates with CGMs. One box of 10 pods – which you need monthly – costs $772 to $808 retail. That’s $9,264 to $9,696 per year just for the plastic pods that go on your body.
Now, pump users CAN access the same $99/month Novo Nordisk program that MDI users get – that’s the good news. The bad news? Pumps waste LOTS of insulin.
When you change a reservoir or pod, there’s insulin left in the old one. When a site fails – and they do fail, from kinks, occlusions, or dislodgement – you waste whatever insulin was delivered to scar tissue instead of your bloodstream. When you prime tubing or fill a new pod, that’s insulin down the drain. Studies estimate pumps waste about 10% more insulin than MDI just from these mechanical losses.
Then add lipohypertrophy – which we’ll get to – and you’re looking at needing 10-20% more insulin to achieve the same blood glucose control. So while you’re paying the same $99/month base rate, you’re burning through vials faster.
Real-world insulin cost for pumps: a minimum of $1,400 to $1,600 annually once you factor in waste.
Add your CGM ($1,200-3,600), routine visits that are more expensive because pump patients need more monitoring ($500-800), and suddenly you’re looking at $12,364 to $15,696 per year for Omnipod 5.
Medtronic, Tandem, and iLet pumps are slightly cheaper on consumables but still run $7,000 to $13,000 annually.
But insurance covers it, right?
Maybe. If you have great insurance, your out-of-pocket might drop to $3,500-6,000 annually (still more than MDI). If you have a high-deductible plan like millions of Americans, you’re eating most of that cost yourself.
Regardless of type or brand of pump selected, you’re always looking at significantly higher costs than multiple daily injections.
THE PROBLEM NOBODY TALKS ABOUT: LIPOHYPERTROPHY
Here’s something the pump companies don’t advertise: LIPOHYPERTROPHY.
Lipohypertrophy (LH) is fatty scar tissue that builds up at infusion sites. It looks like lumps under your skin. And according to studies from 2022-2025, 95% of insulin pump users have it when checked by ultrasound. Only 5% self-report it because most people don’t even know they have it.
Why does this matter?
LH reduces insulin absorption by 20-22%. That means you’re using more insulin to achieve the same blood glucose control. Combined with the mechanical waste from pump operation, you’re looking at a significant increase in insulin consumption.
But it gets worse. LH also increases glucose variability by 52%, which means more highs, more lows, and higher risk of both DKA and severe hypoglycemia – the exact complications the pump was supposed to prevent.
How do you get LH?
Poor site rotation. Using the same spots repeatedly. Leaving infusion sets in too long (more than 2-3 days). Using long cannulas.
How do you prevent it?
Discipline. Rotating sites every 48-72 hours without fail. Getting annual checks with your endocrinologist. Replacing failed sites immediately instead of “just waiting a bit to see if it improves.”
In other words: personal responsibility.
The pump doesn’t manage your diabetes. You do. The pump is a tool. If you use it carelessly, it becomes expensive scar tissue.
Patients want to change their sites less often, that makes sense, but your body and long term LH really determines how often sites should be changed long term. Companies like Tandem are preparing to release sites that claim to last for 7 days (see image below), but do you really want a site to be in the same spot for that long? Not just a “NO” but a “Hell NO.”

THE INSULIN WASTE REALITY
Let’s talk about something MDI users don’t deal with: mechanical insulin waste.
Every time you change a pump reservoir or pod:
You lose whatever insulin remains in the old one (usually at least 10-20 units)
You use insulin to prime the new tubing or pod (5-15 units minimum depending on system)
You waste insulin on failed sites that didn’t absorb properly (whatever is left - between 0 and 200 units or more)
With MDI, you draw exactly what you need. You inject exactly what you drew. The only waste is the occasional drop on your skin or a bent needle you have to replace.
With pumps, waste is built into the system. It’s unavoidable. The manufacturers know it. Your insurance knows it. That’s why pump users typically go through insulin faster despite the $99/month program covering the base cost.
Over a year, that 10% mechanical waste plus potential LH-related increased needs can mean the difference between using 4 vials per month versus 5-6 vials per month. At $99/month for unlimited insulin, you’re covered – but you’re still using significantly more of a precious hormone because of system inefficiency.
Is that waste worth the benefits of pump therapy? For some people, absolutely. For others, it’s throwing away insulin for features they don’t really need.
DO PUMPS ACTUALLY IMPROVE OUTCOMES?
Yes. Sort of. With caveats…
The data shows pumps reduce:
Severe hypoglycemia by 30% (1.5 vs 2.2 events per year)
DKA events by 40% (0.08 vs 0.15 per year)
HbA1c by 0.3-0.5%
Microvascular complications by 10-15% over ten years
Macrovascular events by about 5%
Those are real benefits. Over a lifetime, that translates to thousands in avoided complication costs and meaningful quality-of-life improvements.
BUT… These outcomes assume you’re using the pump correctly. They assume you’re rotating sites, responding to alerts, changing reservoirs on time, and actually engaging with the technology.
If you’re not doing those things, and studies show many pump users aren’t, you’re paying $15,000 a year for outcomes that aren’t materially better than MDI.
I’ve seen pump users with HbA1c levels of 9-10% because they treat the pump like an autopilot. It’s not. It’s a sophisticated tool that requires sophisticated management.
MY 38-YEAR PERSPECTIVE
I started with Regular and NPH injections in 1988. When Humalog came out, I got my first insulin pump in 1994 (a MiniMed - prior name before Medtronic acquisition) – finally, fast-acting insulin that actually worked like it was supposed to. I then used various pumps for the next 20-25 years, though toward the end I was on and off, switching back to MDI periodically when I got tired of dealing with sites and tubing.
In the late 2010s, I went to MDI full-time. For the last few years, I’ve been using Tresiba and Fiasp – a long-acting basal that lasts more than 24 hours and doesn’t have the peaks and valleys of NPH, paired with an ultra rapid-acting bolus insulin. I’ve tried some of the newer pumps – the iLet and Omnipod 5 – as well, but I keep coming back to MDI. My hope was that the more advanced algorithms would adjust automatically based on the amount of LH for a given pump site, but they did not, or they did not allow for tight enough control for my personal standards.
Here’s my honest assessment after spending two+ decades on a pump and several years back on injections:
Pumps are incredible technology when you need them. If you’re having frequent severe lows, if your schedule is wildly unpredictable, if you’re an athlete or have a job that makes MDI impractical, if you’re a parent managing a child’s T1D overnight – pumps can be life-changing. The programmable basal rates alone can be worth it for people with dawn phenomenon or unusual work schedules.
Pumps are expensive overkill when you don’t. If you have a relatively stable schedule, good glucose awareness, and the discipline to inject 4-6 times daily, MDI works perfectly well. I’ve maintained HbA1c levels between 5.6-6.2% on MDI for years. No pump required.
The diabetes industry wants everyone on pumps because that’s where the money is. Your endocrinologist might push pumps because that’s what the guidelines say and that’s what the pharmaceutical reps emphasize. Your diabetes educator might assume you want “the latest technology.”
But here’s what matters: What will you actually use? What can you actually afford? What fits your actual life?
I use MDI currently not because I don’t understand pumps – I used one for 20+ years. Not because I can’t afford one. But because for my current lifestyle, my risk profile, and my management style, MDI works better. Modern long-acting insulins like Tresiba are game-changers compared to the NPH I started with in 1988. Paired with Fiasp, I can achieve the same glucose control I had on a pump without the hassle of site changes, occlusions, and tubing getting caught on door handles. I also use an Eversense CGM which does require a minor surgical procedure to implant, but provides 365 days without needing a site change. I’ll take that consistency any day!
That’s not heroic. That’s what beating natural selection looks like when your pancreas doesn’t work.
THE NATURAL SELECTION FRAMEWORK
Let me be blunt: Without modern medicine, Type 1 diabetics die. Before insulin was discovered in 1921, a T1D diagnosis was a death sentence. You had maybe a year, usually less.
Natural selection doesn’t care about your feelings. It doesn’t care about insurance coverage or endocrinologist recommendations. In the wild, we don’t survive.
But we’re not in the wild. We have insulin. We have technology. We have the ability to manage this condition and live full, productive lives.
The price? Personal responsibility.
Modern pump algorithms and product marketing are steering patients towards allowing the device to do everything for you. You can’t outsource diabetes management to a device, a doctor, or a government program. You have to check your glucose. You have to count your carbs (or at least approximate them reasonably). You have to adjust for exercise, stress, illness, and hormones. You have to rotate injection or infusion sites. You have to refill prescriptions before you run out. You have to keep supplies with you. You have to plan ahead.
Nobody else can do these things for you.
The pump isn’t going to save you if you’re not willing to manage it. MDI isn’t going to save you if you’re not willing to inject consistently. CGM isn’t going to save you if you ignore the alarms.
You beat natural selection by taking responsibility for your life. That’s the lesson 37 years has taught me.
MAKING THE DECISION

So which should you choose? Please GOD do not let the new insulin pump Barbie influence you (see above image and link).
Choose MDI if:
You’re on a tight budget and need to keep costs under $5,000 annually
You’re newly diagnosed and still learning the basics
You prefer simplicity and don’t want to deal with technology
You have good glucose awareness and can maintain decent control with injections
You want to minimize insulin waste
Modern long-acting insulins (Tresiba, Lantus, Levemir) give you the stability you need
You qualify for the Novo Nordisk $99/month program (which you do, regardless of delivery method)
Choose a pump if:
You have frequent severe hypoglycemia or DKA episodes
Your HbA1c is consistently above 7.5% despite good MDI adherence
You need programmable basal rates for dawn phenomenon or shift work
You use CGM and want automated insulin adjustment
You have good insurance that covers most pump costs
You’re committed to rotating sites every 2-3 days without fail
Your lifestyle genuinely benefits from programmable basal rates and bolus options
The convenience benefits outweigh the increased insulin waste
Don’t choose a pump because:
Your doctor said you should
You think it will “make diabetes easier”
You want to be on “the latest technology”
You’re hoping it will magically improve your control without effort
The pump is a tool. Tools require skill. If you’re not willing to develop that skill, you’re wasting money.
THE INSURANCE GAME
If you have employer-sponsored insurance with good prescription coverage, pumps become much more accessible. Your out-of-pocket might be $3,500-6,000 annually, which is manageable for many families.
If you have a high-deductible health plan – and millions of Americans do – you could be facing $7,000-18,000 in out-of-pocket costs before insurance kicks in meaningfully.
If you’re on Medicaid, pump coverage varies wildly by state. Some states cover pumps readily. Others make you jump through hoops proving “medical necessity” even when it’s obvious.
If you’re uninsured or underinsured, MDI is almost certainly your only realistic option unless you can afford to pay cash for everything.
This is the healthcare system we have. It’s not fair. It’s not rational. It’s not designed with patient outcomes as the primary consideration. But it’s reality.
Navigate it strategically. Get your insurance company to put coverage decisions in writing. Appeal denials aggressively. Shop around for pharmacies and use GoodRx or similar programs. Join patient advocacy groups that provide financial assistance.
But understand: nobody owes you a $15,000 insulin pump. I know that’s not what Diabetes Awareness Month messaging says, but it’s true. These are expensive devices. Someone has to pay for them. If insurance won’t, you need to either pay yourself, find assistance, or use a less expensive option.
Personal responsibility means accepting reality and working within it, not demanding someone else solve your problems.
THE LIFETIME COST REALITY
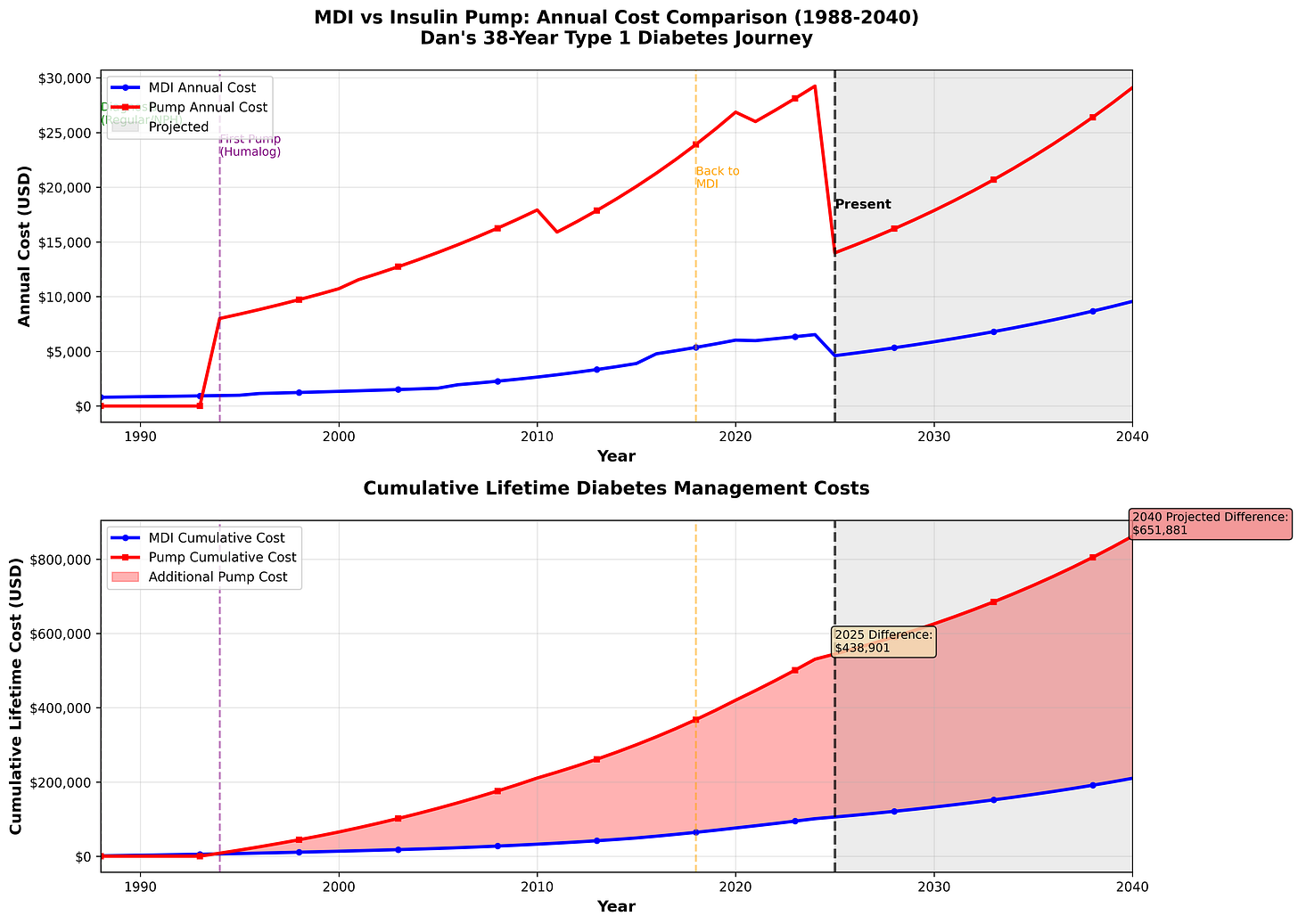
Let me show you what 38 years of diabetes management actually costs.
I created a graph tracking my actual diabetes expenses from 1988 to today, with projections through 2040 based on standard healthcare inflation of 5% annually. The numbers are sobering.
What This Graph Shows:
The top chart shows annual costs over time. Notice how pump costs (red line) jumped dramatically when I got my first pump in 1994 with Humalog. The gap between MDI (blue line) and pump therapy widened consistently until I went back to MDI full-time around 2018.
The bottom chart shows cumulative lifetime costs – the total amount spent managing this disease. The shaded red area represents the additional cost of pump therapy compared to MDI.
The Numbers Don’t Lie:
From 1988 to 2025, if I’d stayed on MDI the entire time, I would have spent approximately $105,000 on diabetes management. But because I used pumps for roughly 20-25 years, my actual spending was closer to $544,000.
That’s an extra $439,000 spent on pump therapy.
That’s not a typo. Four hundred and thirty-nine thousand dollars.
To put that in perspective:
That’s a house in many parts of America
That’s 8-10 years of college tuition
That’s a fully funded retirement account
That’s generational wealth for some families
Was it worth it? For me, during certain periods – YES. When I needed the programmable basal rates, when my schedule was unpredictable, when the technology genuinely improved my quality of life – the extra cost was justified.
But here’s what nobody tells you during Diabetes Awareness Month: you don’t get those years and that money back.
The diabetes industry wants you to believe that choosing MDI over a pump means you’re not taking your health seriously. That’s bullshit. It’s marketing disguised as medical advice.
If the pump delivers value for your specific situation – better control, fewer complications, lifestyle benefits that justify the cost – then it’s worth it. But if you’re on a pump because “that’s what everyone does” or because your doctor pushed it without explaining the alternatives, you’re potentially spending hundreds of thousands of dollars unnecessarily over your lifetime.
Looking Forward:
If current trends continue with 5% annual healthcare inflation, someone diagnosed today will spend over $650,000 more on pump therapy versus MDI over a 50-year period. That number will only grow as device companies add more features, more automation, and more reasons why you “need” the latest model.
Personal responsibility means making informed financial decisions, not just clinical ones. The graph doesn’t lie – pumps cost dramatically more than MDI. Make sure you’re getting value for that difference.
My unCommon Sense
After 37 years, including 20+ years on pumps, here’s what I know:
1. The best diabetes management plan is the one you’ll actually follow. A $15,000 pump you don’t use correctly is infinitely worse than $1,200 worth of insulin pens you inject religiously. I used a pump successfully for two decades. Now I use MDI successfully. The technology isn’t the determining factor, consistency is.
2. Technology is not a substitute for discipline. Pumps, CGMs, smart pens – all amazing tools. None of them replace the fundamental requirement that you pay attention, make adjustments, and take ownership of your health. I’ve had good control on pumps and good control on MDI. The constant? Me doing the work.
3. The diabetes industry profits from complexity. They don’t want you to know that MDI with basic monitoring can work extremely well. They want you thinking you need the latest $10,000 gadget or you’re being irresponsible. That’s marketing, not medicine. Modern insulins like Tresiba and Fiasp are light-years better than Regular and NPH – MDI isn’t the primitive option it was in 1988.
4. Lipohypertrophy is real and it’s expensive. If you use a pump, rotate sites obsessively. Get checked annually. Don’t let scar tissue rob you of the benefits you’re paying thousands for. This was one of the factors that pushed me back to MDI – after two decades of pump use, I had developed significant scar tissue that was affecting absorption.
5. Pumps waste insulin – it’s built into the system. Between priming, failed sites, and LH-related absorption issues, you’ll use more insulin on a pump than on MDI. The $99/month Novo Nordisk program covers both delivery methods, but you’ll burn through vials faster with a pump. After 20 years of pumping, that waste adds up.
6. Cost matters. The medical establishment treats cost discussions as crass or beside the point. But for most Americans, spending an extra $10,000 per year on diabetes management isn’t trivial. That’s a car payment. That’s a college fund contribution. That’s retirement savings. Make sure the benefit justifies the cost for your situation.
7. You can switch methods and be successful. I’m living proof. Pumps aren’t a one-way door. If MDI isn’t working, try a pump. If the pump isn’t working, go back to MDI. Modern insulins have made MDI vastly more effective than it was even 15 years ago.
8. You beat natural selection one decision at a time. Every glucose check. Every carb count. Every injection or bolus. Every site rotation. Every supply order. These aren’t heroic acts. They’re the price of staying alive with a broken pancreas.
I’m alive and healthy 37 years into this diagnosis because I take responsibility. Not because I have the best insurance or the fanciest technology. Not because I’m special or tough or a “diabetes warrior.”
I’m alive because I do the work.
That’s what Diabetes Awareness Month should be about. Not blue ribbons and awareness campaigns and corporate virtue signaling. Awareness is useless without action. Action requires responsibility. Responsibility cannot be transferred to anyone else or to a device (iLet).
If you’re choosing between MDI and a pump this November, ask yourself: Which option will I actually use correctly? Which can I realistically afford? Which fits my life?
Then make the choice and own it.
Your pancreas doesn’t work. That’s not your fault. But managing it? That’s entirely your responsibility.
Nobody else can live your life for you.
If you want to have a constructive conversation about this or anything else, message me at dan@thrailkill.us, and let’s grab coffee or a beer.
Have a good one,
Dan



The breakdown of lipohypertrophy costs really hits home. Most people don't realize that 95% of pump users devlop this issue, and the 20% reduction in insulin absorption is basically lighting money on fire. Your point about site rotation discipline being non-negotiable is crucial, and honestly something I wish more endocrinologists would emphasize upfront. The lifetime cost graph is sobering too, almost half a milion dollars over decades is no joke when you could be investing that diffrential elsewhere.