Vaccines Should Be Questioned, Not Eliminated
Why Choice Should Replace Mandates and Manufacturers need to be Liable to Restore Public Trust
It’s 1988, and I’m a wide-eyed second-grader in South Carolina, suddenly thrust into a world of finger pricks and insulin shots after being diagnosed with Type 1 diabetes. No family history, no clear cause — just a viral infection from my toddler years that may have flipped some autoimmune switch in my body. There was never a causation determined for what caused my type 1 diabetes. Was it vaccines, maybe? Was it a virus triggering an autoimmune reaction, a stronger maybe? Was it other environmental factors, maybe? Would I like to know, sure, but am not going to hold my breath. Fast forward to 2020, and the COVID-19 pandemic hits. As someone who’s spent over three decades managing a chronic condition, I watched the vaccine rollout with a mix of hope and healthy skepticism. I didn’t rush to get the jab—not because I’m anti-vax, but because I’ve learned the hard way that medical decisions aren’t one-size-fits-all. My body, my rules. I also never buy the first model year for a new vehicle so they have time to get the “kinks” worked out., same applies to new therapies.
Now, here we are in September, 2025, and the vaccine debate is hotter than ever. With Robert F. Kennedy Jr. shaking up HHS, recent revelations about misrepresented studies in government documents fueling outrage, and states like Florida eyeing the end of school mandates, it’s a perfect storm for rethinking how we approach vaccines. I’ve written before about my choice not to get the COVID vaccine yet, emphasizing personal responsibility (Thrailkill, 2021). But let’s broaden that: Why should we question vaccines at all? And why ditch mandates? This isn’t about conspiracy theories or fear-mongering—it’s about common sense, choice, and evidence. If mandates are the government’s way of saying “trust us,” remember, they’re the same folks whose recent vaccine docs got caught twisting science according to the latest report.
The History of Vaccine Mandates: From Smallpox to School Requirements
Vaccines have a storied past, saving countless lives since Edward Jenner’s smallpox breakthrough in 1796. In the U.S., mandates kicked off during the Revolutionary War when George Washington ordered his troops variolated against smallpox—basically an early, riskier form of vaccination. It worked; disease ravaged the British but spared many Continentals.
Fast-forward to the 19th century: Massachusetts passed the first state mandate in 1809 for smallpox vaccination, followed by school requirements in 1855. The Supreme Court upheld this in 1905’s Jacobson v. Massachusetts, fining a pastor $5 (about $170 today) for refusing the shot during an outbreak (Jacobson v. Massachusetts, 1905). The court argued public health trumped individual liberty in emergencies, but with limits—no forced injections, just penalties.
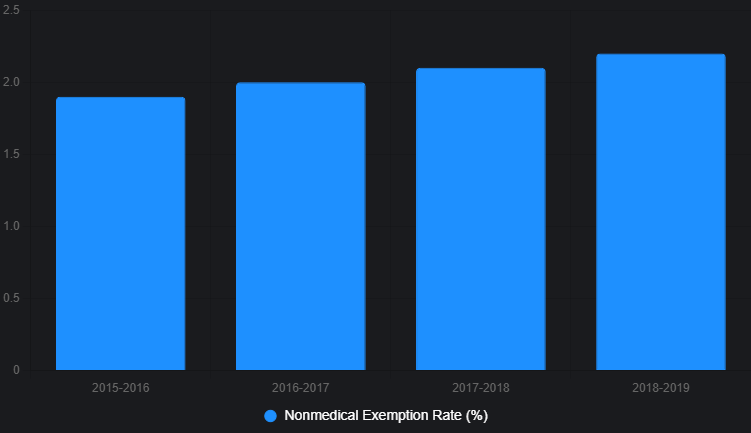
By the mid-20th century, mandates expanded. Polio vaccines in the 1950s led to widespread school requirements, and by 1998-1999, all but four states mandated shots for K-12 entry (Smith et al., 2011). Today, all 50 states require vaccines like measles, mumps, rubella (MMR), and polio for public schools, though exemptions vary: medical in all, religious in 45, and philosophical in 15 (National Conference of State Legislatures, 2025). Yet, nonmedical exemptions are creeping up—2.2% of kindergarteners had them in 2018-2019, a trend the HHS Vaccines National Strategic Plan 2021-2025 flags as a threat to hard-won gains (U.S. Department of Health and Human Services, 2021).
But history shows mandates aren’t infallible. The 1976 swine flu vaccine campaign vaccinated 45 million Americans amid fears of a pandemic that never materialized, leading to 450 cases of Guillain-Barré syndrome—a rare neurological disorder (CDC, 1976). It highlighted rushed rollouts’ risks. Similarly, early COVID mandates faced backlash; by 2025, over 20 states have banned or limited employer mandates, reflecting growing pushback (Jones, 2025).
Mandates were born from necessity, but they’ve evolved into tools that sometimes prioritize compliance over consent. As a diabetic, I’ve questioned every med I’ve taken—why not vaccines?
The Benefits of Vaccines: Undeniable, But Not Absolute
Let’s be clear: Vaccines work wonders. Globally, they prevent 3.5 to 5 million deaths yearly from diseases like diphtheria, tetanus, pertussis, influenza, and measles (World Health Organization, 2024). In the U.S., childhood vaccination rates have eradicated smallpox and nearly wiped out polio. A 2025 CDC report estimates COVID vaccines averted millions of deaths from 2020-2024, reducing hospitalizations by up to 70% in high-risk groups (CDC, 2025a). A meta-analysis reinforces this: COVID shots slashed infection and hospitalization odds, with the most common side effect just being injection-site pain (AFP Fact Check, 2025).
Economically? Huge wins. Vaccines save billions in healthcare costs—averted medical expenses alone make them a no-brainer for societies (Bloom et al., 2023). For kids, 2024-2025 data shows flu and COVID shots cut emergency visits by 40-60%, with no new safety flags (CDC, 2025b). The HHS plan notes that high vaccination rates have kept diseases like measles at bay, with coverage goals aiming for 95% for MMR to maintain herd immunity (U.S. Department of Health and Human Services, 2021).
But benefits aren’t universal. Efficacy varies: The 2024-2025 COVID vaccine is about 54% effective against symptomatic infection but also has a myriad of possible side effects (CDC, 2025c). Do we really want spike proteins being produced by our body that cause inflammation in major systems? I do not. And herd immunity? It requires 95% coverage for measles, but lower for others. Vaccines aren’t magic bullets—they’re tools, best used thoughtfully. The HHS plan warns that falling rates—down 2-3% nationally—risk outbreaks, yet mandates alone aren’t closing the gap (U.S. Department of Health and Human Services, 2021).
The Risks and Side Effects: Rare, But Real Reasons to Question
No medical intervention is risk-free. Common vaccine side effects include soreness, fever, or fatigue—mild stuff affecting 1-2% severely (CDC, 1976). But rarer issues exist: Anaphylaxis hits about 1 in a million doses, and myocarditis from mRNA COVID vaccines affects 1 in 10,000 young males, mostly resolving quickly (Oster et al., 2025) while others, like me, have more long term, lingering symptoms. The HHS plan calls serious adverse events “exceedingly rare,” monitored via systems like VAERS and the Vaccine Safety Datalink, which covers nearly 10 million patients (U.S. Department of Health and Human Services, 2021).
Questioning comes from history. The Cutter Incident in 1955 saw faulty polio vaccines paralyze 200 kids (Offit, 2005). More recently, 2025 studies reaffirm COVID vaccines’ safety but note long-term data gaps—neurological risks like Guillain-Barré persist at low rates (1-2 per million) (Oster et al., 2025). A JAMA article from August 2025 stresses balancing benefits and risks, especially culturally where trust erodes (Smith & Jones, 2025).
As someone possibly virus-triggered into diabetes, I question: Could vaccines alter immunity long-term? Evidence is thin, but French virologist Luc Montagnier warned in 2021 (echoed in 2025 debates) of potential variant risks from mass vaccination (Montagnier, 2021). Not alarmist, just prudent—questioning ensures better science. And when government docs start twisting study results to downplay risks—like claiming higher miscarriage rates that experts say don’t exist—it only amps up the skepticism (AFP Fact Check, 2025).
Restoring Trust Through Accountability: Ending Manufacturer Immunity
If we’re serious about questioning vaccines and rebuilding public trust, we can’t ignore the elephant in the room: manufacturer liability. Since the 1986 National Childhood Vaccine Injury Act (NCVIA), vaccine makers have enjoyed broad immunity from lawsuits for injuries caused by their products (CDC, 1976). This was meant to prevent shortages by shielding companies from crippling lawsuits, but critics argue it’s backfired, reducing incentives for rigorous safety testing and eroding public confidence (Kennedy, 2025).
The NCVIA created the National Vaccine Injury Compensation Program (NVICP), a no-fault system funded by a tax on vaccines, where injured parties seek compensation from the government instead of suing manufacturers directly. While this has paid out billions, it’s criticized for being slow, adversarial, and underfunded—claimants win only about 1 in 4 cases, often after years of litigation (Johnson, 2025). For COVID vaccines, the PREP Act (2005) extended even broader protections, making it nearly impossible to sue for side effects.
This immunity doesn’t just shield Big Pharma; it trickles down to coerce physicians too. As Dr. Brooke Miller recounts in a recent Brownstone Institute piece, doctors who questioned COVID protocols—like mask mandates or Remdesivir—faced firing or professional destruction, turning medicine from a calling into a corporate script (Miller, 2025). “Physicians who dared to think independently... faced professional destruction. The message was clear: conform or be destroyed,” she writes. Mandates didn’t just pressure patients; they silenced healers, fracturing the sacred doctor-patient bond and deepening distrust.
Why end this immunity? First, accountability drives better products. Without the threat of lawsuits, companies might cut corners on long-term safety studies—echoing my own viral-triggered diabetes, where unknown long-term effects changed my life forever. As one petition argues, removing immunity would “end protectionism” and force manufacturers to prioritize safety over profits, potentially leading to fewer injuries and more trust (Kennedy, 2025). The HHS plan stresses better safety monitoring like VAERS, where manufacturers must report all adverse events, but without liability, what’s the real incentive to dig deeper? (U.S. Department of Health and Human Services, 2021).
Second, it restores public faith. Vaccine hesitancy is now a top-10 global health threat, per WHO, amplified by social media misinformation and, lately, questionable government docs (World Health Organization, 2024). In 2025, with RFK Jr. at HHS, there’s momentum: Congress is considering repealing PREP Act protections, and the VITAL Act of 2025 aims to increase transparency and liability in trials to deter shortcuts (Brown, 2025; Kennedy, 2025). RFK Jr. has even pushed to overhaul the NVICP, arguing the current system hides injuries and breeds skepticism (Johnson, 2025). Take the recent HHS memo to lawmakers: It cited studies to justify dropping routine COVID shots for pregnant folks and healthy kids, but experts like Maria Velez from McGill blasted it for flipping her findings—her research actually showed no increased miscarriage risk post-vax (AFP Fact Check, 2025). ACOG’s Steven Fleischman called it out: “The decision was not made based on any new research or latest scientific evidence,” sowing needless doubt (AFP Fact Check, 2025).
From my view, immunity is corporate welfare—subsidizing profits at the expense of individual rights. Ending it wouldn’t ban vaccines; it’d make them safer through market forces. As someone who’s navigated chronic illness, I know trust comes from transparency, not shields. If companies face real consequences, they’ll innovate responsibly, and public buy-in could soar—especially when even HHS docs get fact-checked for falsehoods.
Current Events: The 2025 Mandate Meltdown
September 2025 is mandate mayhem. Robert F. Kennedy Jr.’s Advisory Committee on Immunization Practices (ACIP) panel—stacked with skeptics—voted against the combined MMRV vaccine for kids, delaying hepatitis B newborn shots amid safety debates (Kennedy, 2025; Brown, 2025). Florida plans to phase out school mandates, inspiring other states; anti-vax attorneys call them “bullying tools” (Johnson, 2025). And that HHS memo? It’s the latest spark, with experts decrying its cherry-picked data on myocarditis (mild cases that resolve fast) and ignoring how vax reduced youth hospitalizations (AFP Fact Check, 2025).
West Coast states formed the Western States Alliance, issuing independent guidelines distrusting federal ones post-Trump politicization (Western States Alliance, 2025). Childhood vaccination rates are falling—down 2-3% nationally—fueling religious exemption debates (Kennedy, 2025). A Stat News piece highlighted adviser Martin Kulldorff demanding public debates for trust (Kulldorff, 2025). Meanwhile, the HHS plan warns that anti-vax vocalism, supercharged by social media, threatens decades of progress—yet their own docs aren’t helping by misquoting safety studies (U.S. Department of Health and Human Services, 2021; AFP Fact Check, 2025).
These events scream: Mandates breed division. With the FDA revoking COVID Emergency Use Authorizations (EUAs) in August 2025, shifting to full approval, questions linger on transparency (FDA, 2025). As a parent, I weigh this for my family—choice over coercion (Thrailkill, 2020).
Chart: Decline in U.S. Childhood Vaccination Rates (2020-2025)
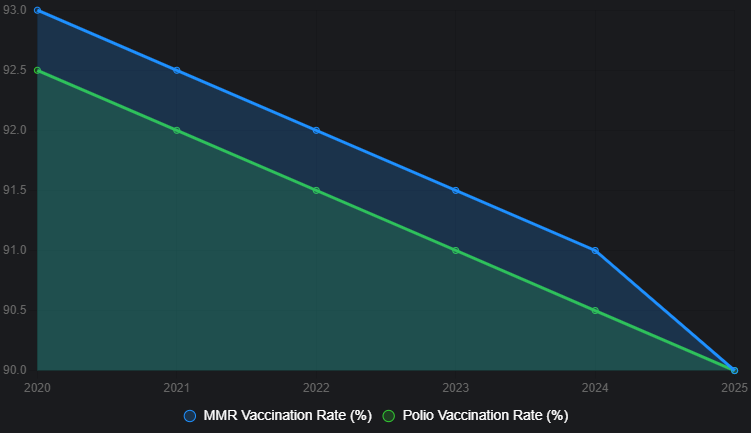
Table: U.S. Kindergarten Nonmedical Exemption Rates (2015-2019)
My unCommon Sense
Vaccines are tools, not talismans. Question them because blind faith in any med invites errors—I’ve questioned insulin doses daily for 37 years (Thrailkill, 2018). Have I stopped taking insulin, no. But are there any long term studies on the non-diabetic complication associated side effects, no. Mandates strip choice, assuming government knows best for your body. But individual responsibility trumps that: You research, weigh risks/benefits, decide. If you’re high-risk, vaccinate. If not, opt out without penalty.
Mandates are like forcing kale on everyone because it’s “healthy”—great for some, gag-worthy for others. And when HHS memos misquote miscarriage studies to push policy? That’s not building trust; that’s building bunkers. My Solutions… End mandates, boost education/transparency. Fund independent studies, make data accessible. Empower parents with exemptions, not exemptions from thinking. And crucially, strip manufacturer immunity—let accountability foster safer products and genuine trust, as RFK Jr.’s reforms suggest (Kennedy, 2025). The HHS plan gets it half-right by calling out disinformation, but until docs stop spreading their own, hesitancy will hover like that 2.2% exemption rate—small now, but snowballing.
To rebuild the doctor-patient bond mandates shattered, consider models like Direct Primary Care (DPC), where docs charge flat fees for unlimited access, ditching insurance bureaucracy. Studies show DPC cuts burnout and boosts outcomes—true choice in action, no corporate overlords scripting shots (Miller, 2025). Physicians like Dr. Miller, fired for bucking protocols, prove it: “Being terminated was one of the most positive things that could have happened to me.” Freedom heals.
This isn’t anti-vax; it’s pro-choice. Nature may have selected me for diabetes but I’ve fought back with decisions (Thrailkill, 2018) that did not always follow the recommendations from my medical professionals. Let folks do the same with vaccines.
I’ve covered history, benefits, risks, current chaos, and the liability angle—now recent HHS drama showing why trust is fracturing. Questioning vaccines sharpens them; mandates and immunity dull trust.
Let’s chat solutions over coffee—maybe we’ll vaccinate the conversation against misinformation.
If you want to have a constructive conversation about this or anything else, reach out to dan@thrailkill.us, and let’s grab coffee or a beer.
Have a good one,
Dan



